Elevating Clinical Outcomes: Innovations for Better Health in the U.S.
Introduction
Value-based care is the healthcare delivery model in which providers, including hospitals and physicians, are financed based on patient health outcomes. Under value-based care agreements, providers are rewarded for assisting patients in enhancing their health, reducing effects and incidence of chronic disease, and living healthier lives in an evidence-based way. Value-based care differs from a fee-for-service or capitated approach, in which providers are paid based on the amount of healthcare services they deliver. The “value” in value-based healthcare is derived from measuring health outcomes against the cost of delivering the outcomes.
The U.S. government has played a vital role in promoting value-based care through initiatives like the Bundled Payments for Care Improvement(BPCI) and the comprehensive Care for Joint Replacement (CJR) models, as well as the persist expansion of ACOs under the Medicare Shared Savings program. Private players, such as insurance companies, have also adopted value-based payment models, further driving the market’s growth.
Value-based Healthcare Benefits
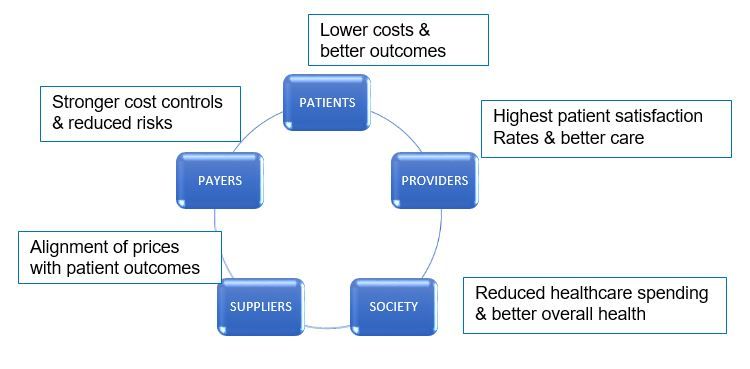
The benefits of a value-based healthcare system extend to patients, providers, payers, suppliers, and society as a whole.
Value-based care helps to treat the patient as a whole person
Value-based care relies greater on integrated care, i.e. health care providers comply together to address a person’s physical, mental, behavioural and social needs. In this way, providers treat an individual as a whole person, rather than focusing on a specific health issue or disease.
Health care teams spend time with individuals receiving value-based care to fully understand:
- Potential obstacles to their care such as access to reliable transportation or healthy food, relationships with family, and general living conditions.
- Their health goals, so their treatment matches up with what they hope to achieve from their health care.
- Providers practicing value-based care help make it more convenient and manageable for people to get care. Providers link individuals to additional resources to best support their health needs and goals, such as through referrals to local social services and programs.
Value-Based Healthcare Translate to New Delivery Models
The burgeon of value-based healthcare is augmenting the care provided by physicians and hospitals. New healthcare delivery models stress a team-oriented approach to patient care and sharing of patient data so that care is coordinated and outcomes can be measured easily.
Value-Based Care Models: Medical Homes
In this, type of model, primary, specialty, and acute care are integrated, often called a patient-centered medical home (PCMH). A medical home is a coordinated approach to patient care, led by a patient’s primary physician who directs a patient’s total clinical care team.
PCMHs cling on the sharing of electronic medical records (EMRs) among all providers on the coordinated care team. The goal of EMRs is to put crucial patient information at each provider’s fingertips, allowing individual providers to see results of tests and procedures performed by other clinicians on the team. This data sharing has the potential to reduce redundant care and associated costs.
Value-Based Care Models: Accountable Care Organizations
Accountable care organizations (ACOs) were originally designed by the Centres for Medicare & Medicaid Services (CMS) to provide high-quality medical care to Medicare patients. In an ACO, doctors, hospitals, and other healthcare providers work as a networked team to deliver the best possible coordinated care at the lowest possible cost. Each member of the team shares both risk and reward, with incentives to improve access to care, quality of care, and patient health outcomes while reducing costs. This approach differs from fee-for-service healthcare, in which individual providers are incentivized to order more tests and procedures and manage more patients in order to get paid more, regardless of patient outcomes.
Direct Contracting Rules for Value-Based Care in US Market
CMS ordained Direct contracting rules in 2021, incentivizing value-based care by linking earnings and losses to the quality of care and patient outcomes. Value-based care has implications for healthtech, because providers can leverage technology to rein in costs. With better data and predictive modelling, physicians can intervene proactively and improve patients’ health, thereby keeping costs low and improving their practices’ profitability. Some start-ups are showing interests in developing infrastructure for value-based care and risk-based models creating a growing area in venture capital (VC) as investors respond to a market opportunity created by the new regulatory environment. Patient engagement portals and dashboards, combined with remote patient monitoring, can help physicians treat patients at a lower cost.
Conclusion
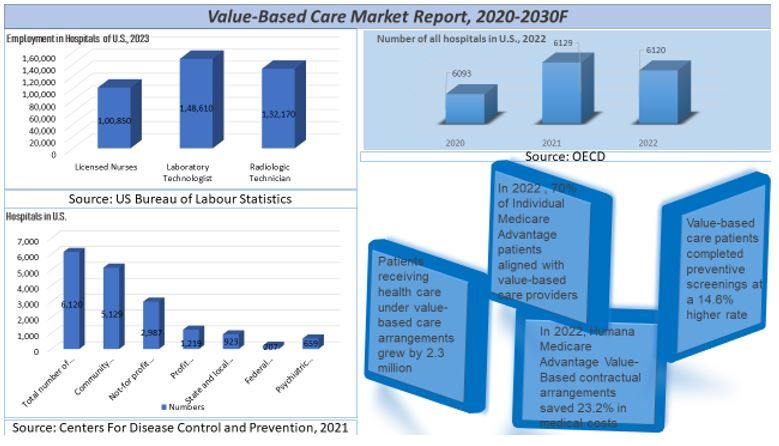
In conclusion, the value-based care market in the U.S. continues to gain traction, driven by efforts to improve patient outcomes, reduce costs, and enhance care delivery. With increasing adoption by payers, providers, and government initiatives, such as alternative payment models and quality incentive programs, the value-based care landscape is poised for further growth and innovation.
The value- based care market in the U.S. is experiencing significant growth and transformation driven by the increasing need to control rising healthcare costs while improving patient outcomes and quality of care. The shift from the traditional fee-for-service model to alternative payment structures, such as bundled payments, accountable care organizations (ACOs), and pay-for-performance programs, is gaining momentum as healthcare providers and payers align their incentives towards delivering value-based care. According to the UnivDatos Market Insights, growing demand of bundled payments will drive the global scenario of the “Value-based care report”. Value-based care market was valued at USD 2.88 billion in 2022, growing at a CAGR of 20.03 % during the forecast period from 2023 – 2030 to reach USD 12.4 billion by 2030.
