美國人口健康管理解決方案市場:當前分析與預測(2025-2033)
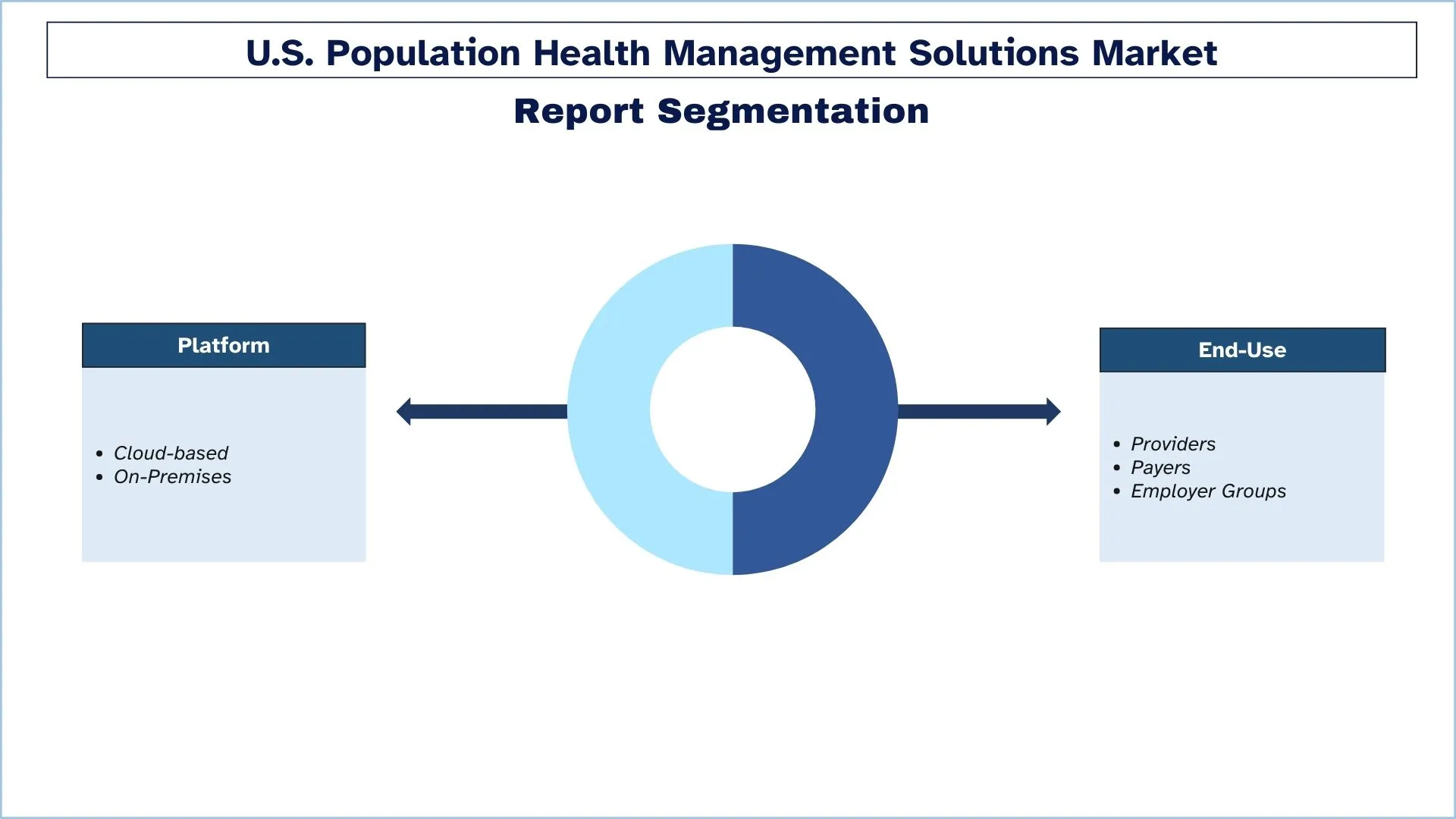
著重於平台(雲端與內部部署);最終用途(提供者、付款人、雇主團體);以及州
美國人口健康管理解決方案市場規模與預測
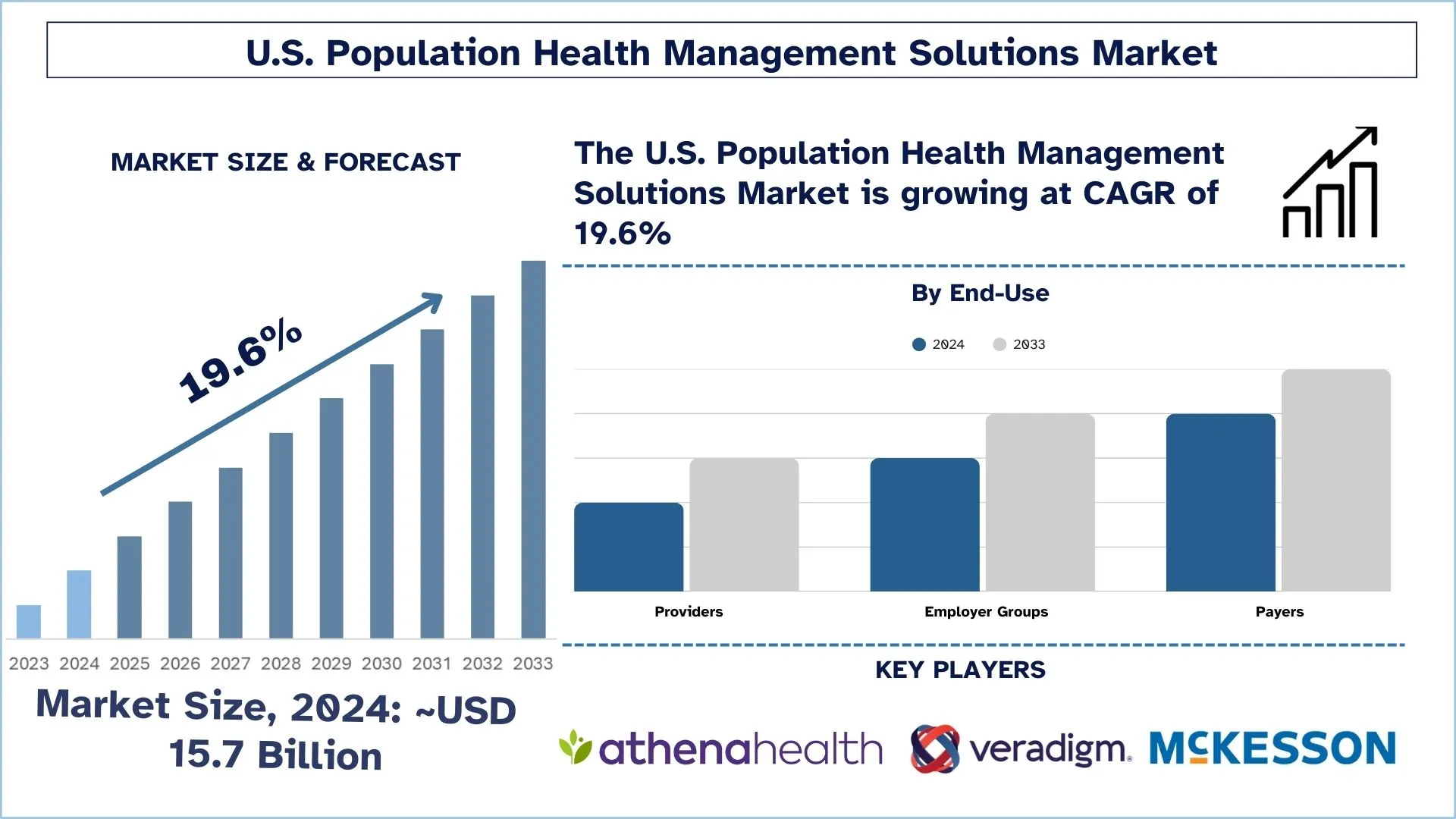
美國人口健康管理解決方案市場於2024年估值約為157億美元,預計在預測期間(2025-2033年)將以約19.6%的顯著複合年增長率增長,這歸因於慢性病負擔增加和人口老齡化。
美國人口健康管理解決方案市場分析
美國的人口健康管理解決方案市場是一個快速增長的行業,其重點是利用技術和數據分析來改善患者群體的健康和福祉。人口健康管理解決方案旨在幫助醫療保健提供者管理患者群體、識別高風險患者,並提供適當的護理以改善患者的預後。美國的人口健康管理解決方案市場受到多種因素的驅動,包括慢性病患病率的增加、管理醫療保健成本的需求以及對遠程患者監護和遠程醫療服務日益增長的需求。人口健康管理解決方案可以幫助醫療保健提供者管理患者群體、識別高風險患者,並提供適當的護理以改善患者的預後。
美國人口健康管理解決方案市場趨勢
本節討論了影響美國人口健康管理解決方案市場各個細分市場的關鍵市場趨勢,這些趨勢由我們的研究專家確定。
轉向基於價值的醫療模式
美國市場的人口健康管理解決方案正在經歷一場徹底的變革,因為醫療保健組織正在轉向基於價值的醫療模式,而不是傳統的基於數量的模式。醫療保健提供者和付款人對 PHM 平台的興趣增加,因為這種趨勢側重於提供預防性護理和更好的患者結果,以及提高成本效益。這些解決方案有助於進行實時分析,將患者劃分為不同的群體,並管理協調護理,同時滿足基於價值的報銷要求。目前,各組織將投資重點放在人口級工具以及風險管理系統和個性化護理解決方案上,以滿足以價值為中心的醫療保健系統內不斷增長的需求。
美國人口健康管理解決方案產業細分
本節提供了對美國人口健康管理解決方案市場報告各細分市場的關鍵趨勢分析,以及2025-2033年的區域層面預測。
雲端細分市場佔據美國人口健康管理解決方案市場的最大份額。
基於平台,市場分為雲端和內部部署。其中,在預測期內,雲端細分市場預計將在美國人口健康管理解決方案市場中佔據主要份額。雲端解決方案提供了優於內部部署解決方案的幾個優點,包括較低的預付成本、可擴展性和更易於維護。雲端解決方案可以根據用戶的需求輕鬆擴大或縮小規模,並且提供商負責維護基礎設施,這可以為醫療保健提供者節省時間和資源。雲端解決方案提供了更大的靈活性和可訪問性,因為可以通過任何有互聯網連接的地方訪問它們。這對於可能難以獲得醫療保健提供者的農村和偏遠地區尤其重要。
付款人細分市場預計將見證比美國人口健康管理解決方案市場更高的複合年增長率。
根據最終用途,市場細分為提供者、付款人和雇主團體。其中,預計在預測期內,付款人將在美國人口健康管理解決方案市場中佔據主要份額。付款人細分市場將在預測期內佔據市場的主要份額。付款人,例如健康保險公司和政府機構,在人口健康管理中發揮著關鍵作用,因為他們負責資助醫療保健服務。付款人對能夠幫助降低醫療保健成本、改善患者預後和增加獲得護理機會的人口健康管理解決方案感興趣。
加州在2024年擁有 значительная 的市場份額。
加州的人口健康管理 (PHM) 解決方案市場經歷 значительная 的變化,原因是州級努力改善健康服務和患者預後。衛生保健服務部 (DHCS) 通過其 CalAIM 計劃啟動了人口健康管理計劃。Medi-Cal 成員的人口健康管理計劃提供了一種完整的個性化健康方法,該方法側重於更好的結果和所有人群(包括兒童、孕婦、老年人和殘疾人)的平等治療機會。這項倡議表明了加州致力於將護理管理系統與患者參與工具和電子健康記錄結合起來,以建立統一的醫療保健結構。對預防醫學的重視,以及對差異解決方案的重視,將使加州成為人口健康管理的典範,以創建一個高效、公平的醫療保健系統。
美國人口健康管理解決方案產業競爭格局
美國人口健康管理解決方案市場具有競爭力,有多家全球和國際參與者。主要參與者正在採取不同的增長策略來增強其市場佔有率,例如合作夥伴關係、協議、合作、新產品發布、地域擴張以及兼併和收購。
美國頂級人口健康管理解決方案公司
一些主要市場參與者包括 Veradigm Inc.; Cerner Corp. (Oracle); Conifer Health Solutions, LLC (Tenet Healthcare); EClinicalWorks; Enli Health Intelligence (Cedar Gate); McKesson Corp.; Medecision (Health Care Service Corporation (HCSC)); Optum, Inc. (UnitedHealth Group); Koninklijke Philips N.V.; athenahealth, Inc. (Bain Capital and Hellman & Friedman)
美國人口健康管理解決方案市場的最新發展
2022年4月,Medecision,數字護理管理領域的領先者,宣布與 Clearstep Health 啟動戰略合作夥伴關係,旨在為現有和新的健康計劃和系統開創增強的患者參與。
美國人口健康管理解決方案市場報告範圍
報告屬性e | 詳細信息 |
基年 | 2024 |
預測期 | 2025-2033 |
增長動力 | 以19.6%的複合年增長率加速增長 |
2024年市場規模 | 157億美元 |
主要貢獻地區 | 預計加州在預測期內的複合年增長率最高。 |
涵蓋的關鍵區域 | 加州、紐約州、佛羅里達州、華盛頓州、德克薩斯州、美國其他地區 |
公司概況 | Veradigm Inc.; Cerner Corp. (Oracle); Conifer Health Solutions, LLC (Tenet Healthcare); EClinicalWorks; Enli Health Intelligence (Cedar Gate); McKesson Corp.; Medecision (Health Care Service Corporation (HCSC)); Optum, Inc. (UnitedHealth Group); Koninklijke Philips N.V.; athenahealth, Inc. (Bain Capital and Hellman & Friedman) |
報告範圍 | 市場趨勢、驅動因素和限制因素;收入估計和預測;細分市場分析;供需方分析;競爭格局;公司概況 |
涵蓋的細分市場 | 按平台、按最終用途、按地區/國家 |
購買美國人口健康管理解決方案市場報告的原因:
該研究包括經過驗證的權威行業專家驗證的市場規模和預測分析。
該報告快速概覽了整體行業的表現。
該報告涵蓋對主要行業同行的深入分析,主要側重於關鍵業務財務、產品組合、擴張策略和近期發展。
對行業中存在的驅動因素、限制因素、關鍵趨勢和機會的詳細考察。
該研究全面涵蓋了不同細分市場的市場。
行業的深度區域級別分析。
定制選項:
可根據需求或其他細分市場進一步定制美國人口健康管理解決方案市場。除此之外,UnivDatos理解您可能擁有自己的業務需求;因此,請隨時與我們聯繫,以獲得完全符合您要求的報告。
目錄
美國人口健康管理解決方案市場分析研究方法(2023-2033)
我們分析了歷史市場,估計了當前市場,並預測了美國人口健康管理解決方案市場的未來市場,以評估其在全球主要地區的應用。我們進行了詳盡的二手研究,以收集歷史市場數據並估計當前的市場規模。為了驗證這些見解,我們仔細審查了大量的調查結果和假設。此外,我們對美國人口健康管理解決方案價值鏈中的行業專家進行了深入的一手訪談。在通過這些訪談驗證了市場數據後,我們使用自上而下和自下而上的方法來預測整體市場規模。然後,我們採用市場細分和數據三角剖分方法來估計和分析行業細分市場和子細分市場的市場規模。
市場工程
我們採用數據三角剖分技術來最終確定整體市場估計,並為美國人口健康管理解決方案市場的每個細分市場和子細分市場得出精確的統計數據。我們通過分析各種參數和趨勢(包括平台、最終用途和美國人口健康管理解決方案市場內的地區)將數據劃分為多個細分市場和子細分市場。
美國人口健康管理解決方案市場研究的主要目的是
該研究確定了美國人口健康管理解決方案市場的當前和未來趨勢,為投資者提供戰略見解。它突出了區域市場的吸引力,使行業參與者能夠開拓尚未開發的市場並獲得先發優勢。研究的其他量化目標包括:
市場規模分析:按價值(美元)評估美國人口健康管理解決方案市場及其細分市場的當前和預測市場規模。
美國人口健康管理解決方案市場細分:該研究按平台、最終用途和地區對市場進行細分。
監管框架與價值鏈分析:檢查美國人口健康管理解決方案行業的監管框架、價值鏈、客戶行為和競爭格局。
區域分析:對加利福尼亞州、紐約州、佛羅里達州、華盛頓州、德克薩斯州、美國其他地區等關鍵地區進行詳細的區域分析。
公司概況與增長策略:美國人口健康管理解決方案市場的公司概況以及市場領導者為維持快速增長的市場而採用的增長策略。
常見問題 常見問題
Q1: 美國人口健康管理解決方案市場目前的規模和增長潛力為何?
截至2024年,美國人口健康管理解決方案市場價值約為157億美元,預計到2033年將以19.6%的複合年增長率增長。
Q2: 美國人口健康管理解決方案市場增長的驅動因素是什麼?
糖尿病、心臟病等慢性病日益普遍,以及人口老齡化,推動了對支持主動、協調護理的PHM解決方案的需求。
Q3: 按最終用途劃分,哪個細分市場在美國人口健康管理解決方案市場中佔據最大份額?
付款人細分市場目前在最終用途細分市場中佔據最大的市場份額。
Q4: 美國人口健康管理解決方案市場的主要趨勢是什麼?
醫療保健提供者越來越多地採用人口健康管理工具來支持基於價值的護理,重點關注預防性護理、患者參與和結果驅動的報銷。
Q5: 哪個地區將主導骨密度測量儀市場?
加利福尼亞州領先美國人口健康管理解決方案市場。
Q6: 美國人口健康管理解決方案市場中最大的挑戰是什麼?
醫療保健系統分散和缺乏標準化的數據格式使得跨提供者整合患者信息變得困難,限制了人口健康策略的有效性。
Q7: 美國人口健康管理解決方案市場中的主要參與者有哪些?
推動美國人口健康管理解決方案創新的領先公司包括:
• Veradigm Inc.
• Cerner Corp. (Oracle)
• Conifer Health Solutions, LLC (Tenet Healthcare)
• EClinicalWorks
• Enli Health Intelligence (Cedar Gate)
• McKesson Corp.
• Medecision (Health Care Service Corporation (HCSC))
• Optum, Inc. (UnitedHealth Group)
• Koninklijke Philips N.V.
• athenahealth, Inc. (Bain Capital and Hellman & Friedman)
Q8: 哪些關鍵的技術創新正在塑造美國人口健康管理解決方案市場?
人工智能驅動的分析、基於雲的平台和實時數據集成等新興技術正在徹底改變PHM解決方案。這些創新使更好的風險分層、預測建模和更個性化、數據驅動的護理計劃成為可能,這些計劃與基於價值的護理模型保持一致。
Q9: 投資者如何評估美國PHM解決方案市場中具有高潛力的機會?
投資者應評估具有可擴展平台、與付款人和提供者建立牢固合作夥伴關係、監管合規性準備以及在護理協調和降低成本方面有實際成果的公司。對人工智能、互操作性和患者參與工具的重點投資提供了巨大的增長潛力。
相關 報告
購買此商品的客戶也購買了